Accountable Care Organizations (ACOs)
What is an ACO?
ACOs are groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high-quality care to their Medicare patients.
The goal of coordinated care is to ensure that patients get the right care at the right time, while avoiding unnecessary duplication of services and preventing medical errors.
When an ACO succeeds both in delivering high-quality care and spending health care dollars more wisely, the ACO will share in the savings it achieves for the Medicare program.
Shared Savings Program
The Medicare Shared Savings Program (Shared Savings Program) offers providers and suppliers (e.g., physicians, hospitals, and others involved in patient care) an opportunity to create an Accountable Care Organization (ACO). An ACO agrees to be held accountable for the quality, cost, and experience of care of an assigned Medicare fee-for-service (FFS) beneficiary population. The Shared Savings Program has different tracks that allow ACOs to select an arrangement that makes the most sense for their organization.
The Shared Savings Program is an important innovation for moving the Centers for Medicare & Medicaid Services’ (CMS’) payment system away from volume and toward value and outcomes. It is an alternative payment model that:
Promotes accountability for a patient population.
Coordinates items and services for Medicare FFS beneficiaries.
Encourages investment in high quality and efficient services.
Are ACOs just a new type of health plan? Not really.
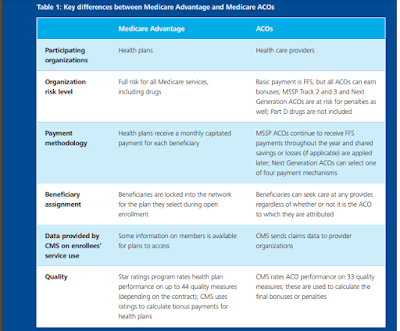
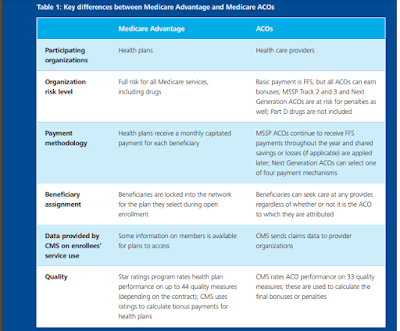
Medicare has three main payment approaches for health care services: FFS, Medicare Advantage, and ACOs.
Under Medicare Advantage, CMS contracts with health plans, which receive a monthly fee to cover services to
beneficiaries. With ACOs, CMS contracts with health care providers, which manage performance risk (i.e., cost
and quality) for a specific patient population. (See Table 1 for key differences between the programs.)
ACO Providers and Suppliers
Eligible ACO providers and suppliers that may participate in the Shared Savings Program include:
ACO professionals in group practice arrangements
Networks of individual practices of ACO professionals
Partnerships or joint venture arrangements between hospitals and ACO professionals
Hospitals employing ACO professionals
Critical Access Hospitals (CAHs) that bill under Method II
Federally Qualified Health Centers (FQHCs)
Rural Health Clinics (RHCs)
Teaching hospitals that have elected to receive payment on a reasonable cost basis for the direct medical and surgical services of their physicians
Care Coordination
Health care providers have reported that a lack of information is a barrier to improving care coordination. While a provider may know about the services they provide to the beneficiary, they often do not know about all the services the beneficiary receives from other health care providers.
To better treat patients and to coordinate their care, Shared Savings Program ACOs may request Medicare claims information about their patients from CMS.
Provider Participation
To participate in the Shared Savings Program, Medicare-enrolled providers and suppliers must form or join an ACO, and the ACO must apply and be accepted to the Shared Savings Program. Providers and suppliers may contact other ACO participants in the region, state, or national professional associations to investigate opportunities to join an ACO. ACOs must have at least 5,000 Medicare fee-for-service (FFS) beneficiaries assigned to their ACO in each benchmark year to be eligible for participation in the Shared Savings Program.
ACO – Other Entities Frequently Asked Questions
Q1. May our practice taxpayer identification number (TIN) affiliate with an Accountable Care Organization (ACO) as an “other entity” instead of as an ACO participant, even though our practice TIN is Medicare-enrolled?
Yes, a Medicare-enrolled entity may enter into an agreement with an ACO as an “other entity.” Regulations governing the Medicare Shared Savings Program (Shared Savings
Program) do not require “other individuals or entities performing functions or services related to ACO activities” to be non-Medicare enrolled individuals or entities.
Q2. If our practice signs an agreement with an ACO as an “other entity,” must our practice be exclusive to a single Shared Savings Program ACO?
No, “other entities” are not required to be exclusive to a single Shared Savings Program ACO. “Other entities” do not appear on the certified ACO Participant List and they would not be used for program operations, such as assignment.
Q3. If our practice signs an agreement with an ACO as an “other entity,” will CMS use our claims to assign beneficiaries to the ACO?
No, CMS does not use claims submitted by an “other entity” that performs functions or services on behalf of an ACO to assign beneficiaries to an ACO. CMS uses only ACO
participants that appear on the certified list submitted by the ACO for program operations, such as assignment or quality reporting sampling. Please review our ACO Participant List and Participant Agreement Guidance regarding changes in ACO participants and ACO providers/suppliers during the performance year to learn about which program operations are dependent on the certified ACO Participant List.
Q4. If our practice signs an agreement with an ACO as an “other entity,” will we qualify for Merit-based Incentive Payment System (MIPS) incentive payments under the Alternative Payment Model (APM) standard through ACO quality reporting?
No, “other entities” do not qualify for a MIPS incentive under the APM scoring standard. Only ACO participants on the certified ACO Participant List can qualify for a MIPS incentive under the APM scoring standard. “Other entities” must participate in MIPS under the regular program, including reporting quality data under one of the available group or individual reporting options.
Performance Year 2021 Medicare Shared Savings Program Accountable Care Organizations – Map
https://data.cms.gov/Special-Programs-Initiatives-Medicare-Shared-Savin/Performance-Year-2021-Medicare-Shared-Savings-Prog/hapm-gazj
Medicare-Medicaid Accountable Care Organization (ACO) Model
Medicare program — and the health care system at large — toward paying providers based on the quality rather than the quantity of care they provide to patients. CMS is adding the Medicare-Medicaid ACO Model to its existing portfolio of ACO initiatives, which include:
Medicare Shared Savings Program (Shared Savings Program)
Pioneer ACO Model
Next Generation ACO Model
ACO Investment Model (AIM)
Comprehensive ESRD Care (CEC) Model