CPT CODE and Description
99244 – Office consultation for a new or established patient, which requires these 3 key components: A comprehensive history; A comprehensive examination; and Medical decision making of moderate complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of moderate to high severity. Typically, 60 minutes are spent face-to-face with the patient and/or family – Average payment – $170 – $200
99245 – Office consultation for a new or established patient, which requires these 3 key components: A comprehensive history; A comprehensive examination; and Medical decision making of high complexity. Counseling and/or coordination of care with other physicians, other qualified health care professionals, or agencies are provided consistent with the nature of the problem(s) and the patient’s and/or family’s needs. Usually, the presenting problem(s) are of moderate to high severity. Typically, 80 minutes are spent face-to-face with the patient and/or family. Average payment – $210 – $250
Office Consultation Codes 99244 and 99245
Procedure Codes 99244 and 99245 require the following key components:
| Level IV – 99244 | Level V – 99245 |
| History – Comprehensive Exam – Comprehensive MDM – Moderate Complexity |
History – Comprehensive Exam – Comprehensive MDM – High Complexity |
As a result of these review findings, a prepayment edit will be implemented on procedure code 99245.
Medical records will be requested to verify that services billed were rendered, medically necessary and billed appropriately to the Medicare program. If the requested medical record documentation is not made available to support services billed, the service may be denied.
Contractors pay for reasonable and medically necessary consultation services when all of the following criteria are met:
- A consultation service is distinguished from other evaluation and management (E/M) visits because it is provided by a physician or qualified non-physician practitioner (NPP) whose opinion or advice regarding evaluation and management of a specific problem is requested by another physician or other appropriate source; and
- A request for consultation from an appropriate source and the need for consultation (i.e., the reason for a consultation service) should be documented by the consultant in the patient’s medical record; and
- After the consultation is provided, the consultant should prepare a written report of his/her findings and recommendations, which must be provided to the referring physician.
For additional information regarding the indications and limitations as well as the documentation requirements for consultation services please refer to Local Coverage Determination, L27484 “Consultations”, located on our website.
Highmark Medicare Services is dedicated to providing education and assisting providers in understanding Medicare regulations. Education on E/M services is provided through many convenient channels including workshops, training modules, and our E/M Center located on our website.
The E/M center can be found on the Part B Homepage. To access this site, click on the “E/M Center” link located on the left-hand side of the page. Please refer to this center in order to access the most current information and educational materials regarding E/M services.
Which Level to Choose
Once you have determined that the visit meets all the criteria to be considered a consult, the next issue is which level to choose. To select the appropriate level consultation code, all three key components (history, examination and medical decision-making) must meet or exceed the requirements stated in CPT®
to qualify for a specific level of E/M service. Refer to the following table:

Choosing the level using Time as the deciding factor
When is it appropriate to choose the level of E/M Consultation based on time? You may choose the level based on time when you have spent greater than 50% of the total time of the visit in counseling or coordination of care for your patient. The guidelines are very clear as to the proper way to document this occurrence. Your note must show the following:
1. Total time of the visit must be documented.
2. The content of the counseling and/or coordination of care must be documented.
3. The note must clearly state that greater than 50% of the total time was spent in counseling and/or coordination of care.
An example of this documentation is as follows: Total visit 30 minutes, 20 minutes spent counseling patient on side ef ects of medication (99242). The times for each level are listed in the table below:
CPT Code Minute
99241 15 Min
99242 30 Min
99243 40 Min
99244 60 Min
99245 80 Min
Evaluation and Management CONSULTATIONS (Codes 99241-99245)
When to Code an Evaluation and Management Service as a Consultation
One of the most frequently asked questions is how to determine if an evaluation and management (E/M) service is a consultation. The discreet difference between a consultation and an office visit is that a consultation is provided by a practitioner whose opinion or advice regarding evaluation and/or management of a specific problem is requested by another practitioner. An office visit is deemed a consultation only when the following criteria for the use of a consultation code are met:
1. Consultation is being performed at the REQUEST of another practitioner or appropriate source requesting advice regarding evaluation and/or management of a specific problem
2. The request for the consultation and the reason for the request must be RECORDED in the patient’s medical record.
3. After the consultation is provided, the practitioner must prepare a written REPORT of his or her findings, which is provided to the referring practitioner.
If all the listed requirements are not met then the appropriate office or other outpatient (99201-99215) or hospital inpatient (99221-99223) E/M service should be reported instead of a consultation code.
Some of the confusion in coding consultations begins with the terms used to describe the requested service. The word ‘consultation’ and the word ‘referral’ are sometimes incorrectly considered one and the same. When a practitioner refers a patient to another practitioner, it cannot be automatically considered a consultation. The service can only be considered a consultation if the above criteria are met in the service provided. A service provided to a patient who was referred to another practitioner without written or verbal request for a consultation (which is documented in the patient’s record) should be coded using one of the office or other outpatient codes or hospital care codes.
The decision to request a consultation is exclusively up to the requesting practitioner. The medical necessity for a consultation is dependent on the clinical judgment of the practitioner. Once the requesting practitioner receives the report from the consulting practitioner, he or she may either continue to manage the patient’s condition or request the consulting practitioner to take over the management of the patient’s condition from that point forward. If the consulting practitioner chooses to accept management of the patient’s condition after the consultation has been completed, the appropriate code from the office or other outpatient or hospital inpatient should be used for any further E/M services provided.
Examples That Do Not Fulfill the Criteria for Consultations:
Standing orders in the medical record for consultations
No order for a consultation
No written report of a consultation
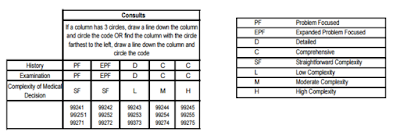
Consults
If a column has 3 circles, draw a line down the column and circle the code OR find the column with the circle farthest to the left, draw a line down the column and circle the code
Consultation and office visit CPT cross walk
CPT Consultation Code Coding Crosswalk New Patient (Requires all three key components) CPT Crosswalk Established Patient (Requires two of three key components)
CPT 99244 As 99204
• A comprehensive history
• A comprehensive examination
• Medical decision making of moderate complexity
As 99214
• A comprehensive history
• A comprehensive examination
• Medical decision making of moderate complexity
CPT 99245 AS 99205
• A comprehensive history
• A comprehensive examination
• Medical decision making of high complexity
AS 99215
• A comprehensive history
• A comprehensive examination
• Medical decision making of high complexity
Billing Bundling Guidelines
99244 to 99214
99245 to 99215
Office Visits – Office services provided on an emergency basis (99058) are considered mutually exclusive to the primary services provided.
Office visit (99211) is considered mutually exclusive to 95115-95117(allergen immunotherapy). Separate reimbursement is not allowed for mutually exclusive services.
Pap Smears – Obtaining a pap smear is integral to the office visit. This includes both preventive and routine office visits. Separate reimbursement is not allowed for Q0091.
Pathologists – Claims submitted by pathologists (provider specialty 29) for clinical interpretation of laboratory results will be allowed for codes 83020, 84165, 84166, 84181, 84182, 85060, 85390, 85576, 86255, 86256, 86320, 86325, 86327, 86334, 86335, 87164, and 87207. Pathology interpretation of all other codes in the 80002-87999 range is considered integral to the laboratory test. Separate reimbursement is not allowed for integral services.
Pulse Oximetry – Pulse oximeters are considered incidental to office visits or procedures. Separate reimbursement is not provided for incidental procedures.
Respiratory Treatments – Demonstration and/or evaluation of patient utilization of an aerosol generator, nebulizer, metered dose inhaler or IPPB devise is considered mutually exclusive to an office visit.
Separate reimbursement is not provided for mutually exclusive services.
Robotic Surgical Systems – Payment for new technology is based on the outcome of the treatment rather than the “technology” involved in the procedure. Additional reimbursement is not provided for the robotic surgical technique.
STAT or After Hours Laboratory Charges – Additional charges for STAT or after hours laboratory services are considered an integral part of the laboratory charge.
Surgical Supplies – Surgical supplies will be considered incidental to Surgical; Laboratory; Inpatient, Outpatient or Office Medical Evaluation and Management; and Consultation services.
Surgical dressings applied in the provider’s office are considered incidental to the professional services of the health care practitioner and are not separately payable. Surgical dressings billed in the provider’s office (place of service 11) will be denied.
Surgical trays and miscellaneous medical and/or surgical supplies are generally considered incidental to all medical, chemotherapy, surgery, and radiology services, including those performed in the office setting.
Supplies (except those related to splinting and casting) are considered components of the 0, 10, and 90- day global surgical package, and are not separately billable on the same date of service as the 0, 10, or 90-day procedure.
Supplies are not covered when they do not require a prescription and can be purchased by the member over-the-counter or when they are given to the member as take-home supplies. Medical and/or surgical supplies, such as dressings and packings, used during the course of an office visit are generally considered incidental to the office visit.
Compression/pressure garments, elastic stockings, support hose, foot coverings, leotards, knee supports, surgical leggings, gauntlets, and pressure garments for the arms and hands are examples of items that are not ordinarily covered.
Transvaginal Ultrasound – Transvaginal ultrasound (76830) is considered mutually exclusive to a hysterosonography with or without color flow Doppler (76831).
Venipuncture – Refer to policy “Code Bundling Rules Not Addressed in Claim Check.”
Vision Services – please refer to CEC’s bundling guidelines related to routine vision services.
X-Rays – When single view and double view chest X-Rays are billed together (71010 and 71020), only the double view X-Ray is allowed. When the entire spine, survey study is billed (72082) with cervical spine films (72040), thoracic spine films (72070) or lumbosacral spine films (72100) only the entire spine, survey study code is allowed. When a single view X-Ray code is billed with a multiple view X-Ray code, only the multiple view X-Ray code is allowed (e.g., 72020 with 72040, 72070, or 72100). Only one professional and one technical component are allowable per X-Ray
Indications
The intent of a consultation service is that a physician or qualified NPP or other appropriate source is asking another physician or qualified NPP for advice, opinion, a recommendation, suggestion, direction, or counsel etc. in evaluating or treating a patient because that individual has expertise in a specific medical area beyond the requesting professional’s knowledge. Consultations may be billed based on time if the counseling/coordination of care constitutes more than 50 percent of the face-to-face encounter between the physician or qualified NPP and the patient. The preceding requirements (request, evaluation (or counseling/coordination) and written report) must also be met when the consultation is based on time for counseling/coordination.
A consultation may not be performed as a split/shared E/M visit.
Consultation Followed By Treatment
A physician or qualified NPP consultant may initiate diagnostic services and treatment at the initial consultation service or subsequent visit. Ongoing management, following the initial consultation service by the consultant physician, should not be reported with consultation service codes. These services should be reported as subsequent visits for the appropriate place of service and level of service. Payment for a consultation service should be made regardless of treatment initiation unless a transfer of care occurs.
Transfer of Care
A transfer of care occurs when a physician or qualified NPP requests that another physician or qualified NPP take over the responsibility for managing the patients’ complete care for the condition and does not expect to continue treating or caring for the patient for that condition.
When this transfer is arranged, the requesting physician or qualified NPP is not asking for an opinion or advice to personally treat this patient and is not expecting to continue treating the patient for the condition. The receiving physician or qualified NPP shall document this transfer of the patient’s care to his/her service in the patient’s medical record or plan of care.
In a transfer of care the receiving physician or qualified NPP would report the appropriate new or established patient visit code according to the place of service and level of service performed and should not report a consultation service.
Reimbursement Guidelines Consultation Services
The American Medical Association (AMA) Current Procedural Terminology (CPT ®) book describes a consultation as a type of evaluation and management service provided at the request of another physician or appropriate source to either recommend care for a specific condition or problem or to determine whether to accept responsibility for ongoing management of the patient’s entire care or for the care of a specific condition or problem.
Services initiated by a patient and/or family and not requested by a physician or other appropriate source should not be reported using CPT consultation codes 99241-99245 or 99251-99255 or HCPCS consultation codes G0406-G0408 or G0425-G0427, but may be reported using appropriate office visit, hospital care, home service or domiciliary/rest home care codes.
UHC Community Plan Medicaid:
UnitedHealthcare Community Plan will consider a claim for a consultation service for reimbursement for Medicaid members if the requesting or referring provider or other appropriate source is identified on the claim. If the requesting or referring entity is not identified on the claim, the consultation service will be denied because it does not meet basic AMA requirements for reporting such a code.
Note: AMA guidelines state that only one inpatient consultation (99251-99255) should be reported by a consultant per admission. Evaluation and Management (EM) services after the initial consultation during a single admission should be reported using non-consultation EM codes. UHC Community Plan Medicare:
Effective January 1, 2010 CMS ceased reimbursing Evaluation and Management (E/M) codes describing consultation services (CPT 99241-99245 and 99251-99255) in all places of service. The codes were assigned a status indicator of “I” beginning with the January 2010 National Physician Fee Schedule (NPFS). Therefore, UnitedHealthcare Community Plan will not reimburse consultation codes 99241 – 99245 or 99251-99255 for Medicare members. HCPCS consultation codes G0406-G0408 or G0425- G0427 will be considered for reimbursement for Medicare members if the requesting or referring provider or other appropriate source is identified on the claim.
BCBS Guideline for different consult service
• Emergency Department Consults: Use the appropriate code from the 99281-99285 series (as directed by CMS) or use the 99201-99215 series with the hospital emergency department site of service code. In all cases the service must be face to face and meet CPT coding rules. In all cases, the services must be face-to-face and meet CPT coding rules.
Inpatient Hospital Consults: For the initial contact in the inpatient setting, the code selection shall be based upon the level of service using CPT definitions for codes 99221-99233. Services were formerly coded with lower level service using subsequent hospital care codes (99231-99233). Do not select codes 99221-99223 based solely upon the service being the first contact for the stay. No physician (or member of the same group who is also in the same specialty) may report an Initial Hospital Care service more than once per stay.
• Nursing Facility Consults: For the initial contact in the nursing facility setting, the code selection shall be based upon the level of service using CPT definitions for codes 99304-99310. This means that services that were formerly coded with lower level consultation codes will be coded using subsequent nursing facility care codes (99307-99310). Do not select codes 99304-99306 based solely upon the service being the first contact for the stay. No physician/professional (or member of the same group who is also in the same specialty) may report an Initial Nursing Facility Care service more than once per stay. Nurse Practitioners (RNP), Physician’s Assistants (PA) and Clinical Nurse Specialists (CNS) may report 99304- 99307 for consultations, so long as a physician in the same clinical field does not report these services.
For example, a PA in a surgical practice and the physician surgeon in that practice may not both report a consultation during the stay. Only physicians may perform the actual admission service, per federal regulations, but non-physician professionals may report 99304-99306 for consultations.
• AI Modifier: We ask the admitting physician to use the AI modifier, Principal Physician of Record.
• Inpatient and outpatient evaluation and management services, same day: As has always been the case, it is not permissible to report both services on the same date.
• Prolonged Services: Use face-to-face time for outpatient services and unit time for inpatient services when determining code selection and service duration. Time spent on teaching rounds or conferences is not counted.
• Coordination of Benefits/Multiple Payers: BCBSRI will not recognize 99241-99245 and 99251- 99255. If BCBSRI is secondary to a payer that does recognize those codes and you wish to use them for the primary payer, we will accept them in the usual manner and crosswalk the submitted codes to the codes we do utilize. Alternatively, you may elect to report services to the primary payer using the methodology BCBSRI uses, if allowed by that payer. The crosswalk was created using key components in CPT.
United Healthcare Update Consultation Codes
** United Healthcare will align with the Centers for Medicare & Medicaid Services (CMS) and no longer reimburse consultation services represented by CPT codes 99241-99245 and 99251-99255.
** This update is effective for claims with dates of service on or after Oct. 1, 2017
** United Healthcare will reimburse the appropriate evaluation and management (E/M) procedure code which describes the office visit, hospital care codes reported in lieu of a consultation services procedure code.
** This notification will be the first of several communications to clarify this change in reimbursement strategy supporting the commitment to the triple aim of improving health care services, health outcomes and overall cost of care.
** Intially when CMS made an original decision to no longer recognize these consultation services procedure codes, United Healthcare began pursuit of data analysis and trending to better understand the use of consultation services codes as reported in the treatment of our commercial members.
** UHC has revealed misuse of consultation services codes by extensive data analysis on consultation codes similar to CMS‟s findings
** The current Relative Value Unit (RVU) assignments reflect numerous changes made during recent years to both E/M codes and other surgical services creating an overall budget neutral experience supporting this strategy as a more accurate reflection of services rendered.
CONSULTATION CROSS WALK CODES
Inpatient (POS 21) Office POS 11/Out Patient (POS 22)
Consults Crosswalk Consults Crosswalk
99251 99221 99241 99201/99212
99252 99221 99242 99202/99213
99253 99221 99243 99203/99213
99254 99222 99244 99204/99214
99255 99223 99245 99205/99215

