Before you appeal a claim or request a redetermination
Before you file an appeal:
1. Have you checked claims status via SPOT or the IVR?
2. Do you have a SPOT account? If not, get one.
3. Was your claim returned as unprocessable? Here’s how to correct it.
4. Have you reviewed the remittance advice to find out why the claim was not paid, or not paid in full?
5. Is there an opportunity to do a clerical reopening?
Issue
Each month, thousands of medical providers send written inquiries to First Coast Service Options Inc. (First Coast) to check the status of an appealed claim. Unfortunately, many of these appeals and subsequent inquiries are submitted on claims that were ineligible for appeal. Because of this, many providers experience a delay in payment and exhaust valuable time as the process of giving each inquiry its due attention can take up to 60 days.
In fact, most of providers in this scenario would have received payment sooner had they used one of First Coast’s web tools before they mailed their request for a redetermination.
Alternative solutions
1. Check the status of the claim and reason codes first
Claims returned as unprocessable cannot be appealed. Unprocessable claims are returned with the MA130 remittance advice message and a corresponding reason code message to denote why the claim was incomplete or invalid. First Coast offers this information for you to resolve this problem.
Before requesting a redetermination (first level of appealing a Medicare claim), check current claims status via SPOT (Secure Provider Online Tool) or the Part B interactive voice response (IVR) system. In addition, review your remittance advice to find out why payment on a claim may have been reduced or denied.
Many claim redetermination requests can be avoided by reviewing the reason for your claim denial to see if you can resubmit the claim through as a clerical reopening.
2. Transposed dates of service and other clerical errors are easily corrected
Correcting information on claims returned as unprocessable (RUC) and resubmitting the claim is one way to avert lengthy delays in payment. Other claim issues can be resolved without having to request a redetermination or appeal. If a claim was accepted then denied, it is possible a clerical error could have occurred such as a transposed procedure or diagnostic code, inaccurate data entry of a provider number, a modifier, or the date of service. These errors can be corrected through a clerical reopening of the claim.
First Coast offers multiple ways to complete a clerical reopening. If you use SPOT, you may be able to correct such information immediately and avoid a delay in payment.
In some cases, a claim may have been denied as a duplicate claim when it would have otherwise been paid had the correct modifier been submitted with it. Here is how one provider used the SPOT to review a denied claim and correct it.
3. Your claim denial may have gotten caught up with a processing issue
As Medicare policy and procedures change, sometimes electronic processing of claims lags behind these policy changes. First Coast reprocesses claims brought to its attention when errors are made in the electronic processing of claims. First Coast offers a sortable table of current processing issues that may have affected the processing of your claim. The table lets you know if any action is required on your part to have a claim reviewed when a processing issue affects it.
4. Check the status of your appeal
Using the First Coast website, you can confirm that First Coast has received your redetermination request. The appeals confirmation search tool allows you to search by your PTAN to confirm your submission has been received by First Coast. Confirming submission can help prevent the filing of duplicate redetermination requests
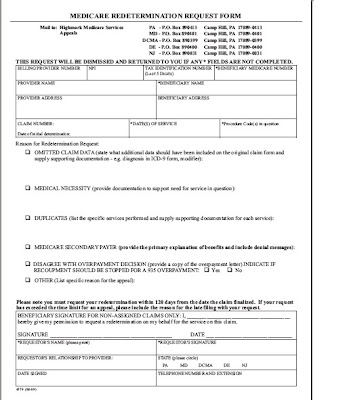
Part B Re-determination Request (Form 4579)