Procedure Code Description Site of Service
77055 Mammography; unilateral Office/Freestanding (Global) 2.52 $90.23 Facility (Professional) 1.00 $35.80 Facility (Technical) 1.52 $54.42
77056 Mammography; bilateral Office/Freestanding (Global) 3.24 $116.01 Facility (Professional) 1.24 $44.40 Facility (Technical) 2.00 $71.61
77057 Screening mammography, bilateral (2-view film study of each breast) Office/Freestanding (Global) 2.31 $82.71 Facility (Professional) 1.00 $35.80 Facility (Technical) 1.31 $46.90
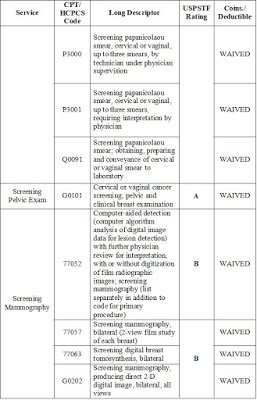
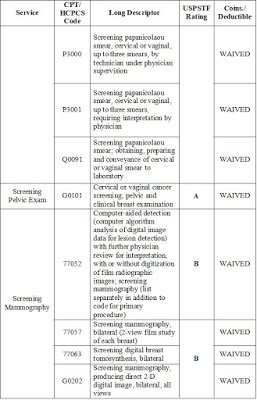
Screening Mammography
Medicare covers one screening mammogram for women aged 40 years or older once every 12 months. CPT code 77057 (screening mammography, bilateral [two view film study of each breast]) is reported if a standard screening mammogram is performed. Medicare also covers computer aided detection (CAD) technology when performed in addition to the standard mammography. This service is reported using CPT add-on code +77052 (computer-aided detection (computer algorithm analysis of digital image data for lesion detection); screening mammography) in addition to code 77057. The Medicare deductible is waived for this service but the patient is responsible for 20% of the Medicare approved amount.
In April 2001, Medicare began to cover and provide additional payment for the use of digital technology for screening and diagnostic mammography studies. HCPCS code G0202 (Screening mammography, producing direct digital image, bilateral, all views) was developed to be reported for a screening full-field digital (FFDM) mammogram. Diagnosis code(s) V76.11 (screening mammogram for high-risk patient) or V76.12 (other screening mammogram) should be linked to the appropriate CPT-4 mammography code reported. The Medicare deductible is waived for this service but the patient is responsible for 20% of the Medicare approved amount.
A diagnostic mammogram (when the patient has an illness, disease or symptoms indicating the need for a mammogram) is covered whenever it is medically necessary.
Computer-Aided Detection (CAD) Add-On Codes
Effective for services on or after January 1, 2002 thr ugh December 31, 2003, (or April 1, 2002 for hospitals subject to OPPS) a new Procedure code 76085, CAD conversion of standard film images to digital images has been established as an add-on code that can be billed only in conjunction with the primary service screening mammography code 76092. The definition of 76085 is: “Digitization of film radiographic images with computer analysis for lesion detection and further physician review for interpretation, mammography (list separately in addition to code for primary procedure).”
NOTE: For claims with dates of service April 1, 2003 – December 31, 2003, code G0202 may be billed in conjunction with 76085.
Carriers and FIs make payment under the Medicare physician fee schedule. There is no Part B deductible. However, coinsurance is applicable.
For claims with dates of service April 1, 2005, and la er, hospitals bill for code 76082* (77051*) under the 13X bill type. The 14X bill type is no longer applicable. Appropriate TOBs for providers other than hospitals are 22X, 23X, and 85X.
Contractors must assure that claims containing code 76085 also contain HCPCS code 76092 or G0202. If not, FIs return claims to the provider with an explanation that payment for code 76085 cannot be made when billed alone. Carriers deny payment for 76085 when billed without 76092 or G0202.
NOTE: When screening CAD 76085 is billed in conjunction with a screening mammography (76092 or G0202) and the screening mammography (76092 or G0202) fails the age and frequency edits in CWF, both services will be rejected by CWF.
Effective with claims with dates of service January 1, 2004 thru December 31, 2006, HCPCS code 76083, “Computer aided detection (computer algorithm analysis of digital image data for lesion detection) with further physician review for interpretation with or without digitization of film radiographic images; screening mammography (list separately in addition
to code for primary procedure),” can be billed in conjunction with the primary service mammography code 76092 or G0202.
Effective with claims with dates of service January 1, 2007 and later, HCPCS code 77052, which replaces code 76083 “Computer aided detection (computer algorithm analysis of digital image data for lesion detection) with further physician review for interpretation with
or without digitization of film radiographic images; screening mammography (list separately in addition to code for primary procedure),” can be billed in conjunction with the primary service mammography code 77057 or G0202.
Contractors must assure that claims containing code 77052* (76083*) also contain HCPCS code 77057* (76092*) or G0202. FIs return claims containing code 77052* (76083*) that do not also contain HCPCS code 77057* (76092*) or G0202 with an explanation that payment for code 77052* (76083*) cannot be made when billed alone. Carriers deny payment for 77052* (76083*) when billed without 77057* (76092*) or G0202.
NOTE: When screening CAD 77052* (76083*) is billed in conjunction with a screening mammography (77057* (76092*) or G0202) and the screening mammography (77057* (76092*) or G0202) fails the age and frequency edits in CWF, both services will be rejected by CWF. *For claims with dates of service prior to January 1, 2007, providers report Procedure codes 76083 and 76092 or G0202. For claims with dates of service January 1, 2007 and later, providers report Procedure codes 77052 and 77057 or G0202, respectively.
Diagnostic Add-on Codes G0236 and 77051* (76082*) Effective for services on or after January 1, 2002 thru December 31, 2003, (or April 1, 2002 for hospital claims subject to OPPS), HCPCS code G0236 was established for diagnostic mammography CAD that can be billed only on the same claim with the primary service of either 76090 or 76091. The definition of G0236 is: “Digitization of film radiographic images with computer analysis for lesion detection and further physician review for interpretation.”
The code must be listed separately in addition to code for the primary procedure.
NOTE: For claims with dates of service April 1, 2003 – December 31, 2003, code G0204 and G0206 may be billed in conjunction with G0236.
For claims with dates of service April 1, 2005, and later, hospitals bill for code 76082* (77051*) under the 13X bill type. The 14X bill type is no longer applicable. Appropriate TOBs for providers other than hospitals are 22X, 23X, and 85X.
There are no frequency limitations on film or digital diagnostic tests or CAD-diagnostic tests. Contractors must assure that claims containing code G0236 also contain HCPCS code 76090, 76091, G0204, or G0206. If not, FIs return claims to the provider with an explanation that payment for code G0236 cannot be made when billed alone. Carriers deny payment for G0236 when billed without 76090, 76091, G0204, or G0206.
Effective with claims with dates of service January 1, 2004 thru December 31, 2006, HCPCS code 76082, “Computer aided detection (computer algorithm analysis of digital image data for lesion detection) with further physician review for interpretation with or without digitization of film radiographic images; diagnostic mammography (list separately in ddition to code for primary procedure),” can be billed in conjunction with the primary service mammography code 76090, 76091, G0204, or G0206.
Effective Date: January 1, 2007
Implementation Date: January 2, 2007
I. GENERAL INFORMATION
A. Background: New 2007 Current Procedural Terminology (CPT) mammography codes have been assigned for screening and diagnostic mammography services. These codes will replace the current CPT codes; however the CPT code descriptors for the services are unchanged.
B. Policy: : Effective for claims with dates of service January 1, 2007 and later, providers report new CPT codes 77051, 77052, 77055, 77056, and 77057 in place of current CPT codes 76082, 76083, 76090, 76091, and 76092 respectively.
II. BUSINESS REQUIREMENTS Use “Shall” to denote a mandatory requirement Number Requirement Responsibility (place an “X” in each applicable column) SharedSystem
5327.1 Upon release of the 2007 CPT codes by the American Medical Association (AMA), contractors shall advise providers that effective for claims with dates of service January 1, 2007 and later, the following new CPT codes have been assigned to mammography services:
77051 77052 77055 77056 77057
The CPT code descriptors for the services are unchanged.
X X X 5327.2 Contractors shall advise providers to report new X X X
Number Requirement Responsibility (place an “X” in each applicable column) SharedSystem codes for mammography claims effective January 1, 2007 as follows:
• report code 77051 in place of code 76082;
•report code 77052 in place of code 76083;
• report code 77055 in place of code 76090;
• report code 77056 in place of code 76091;
• report code 77057 in place of code 76092;
5327.2.1 Contractors shall use the following type of service (TOS) for the new codes:
77051—TOS 4
77052—TOS 1
77055—TOS 4
77056—TOS 4
77057—TOS 1
X X X 5327.3 Contractors shall return to providers claims with dates of service on or after January 1, 2007, containing CPT codes 76082, 76083, 76090, 76091, or 76092. X X X X X OPPS/ OCE
5327.4 Contractors and CWF shall update their systems to discontinue CPT codes 76082, 76083, 76090, 76091, and 76092 and replace them with new CPT codes 77051, 77052, 77055, 77056, and 77057 respectively. X X X X X X
5327.5 Contractors shall update any edits in their systems that contain CPT codes 76082, 76083, 76090, 76091, 76092 to replace them with CPT codes 77051, 77052, 77055, 77056, and 77057 respectively. X X X X X X
5327.6 CWF shall apply existing frequency standards for new screening mammography CPT codes 7052 and 77057 effective January 1, 2007. X
J. Breast (Incision, Excision, Introduction, Repair and Reconstruction)
1. Since a mastectomy (CPT codes 19300-19307) describes removal of breast tissue including all lesions within the breast tissue, breast excision codes (19110-19126) generally are not separately reportable unless performed at a site unrelated to the mastectomy. However, if the breast excision procedure precedes the mastectomy for the purpose of obtaining tissue for pathologic examination which determines the need for the mastectomy, the breast excision and mastectomy codes are separately reportable.
(Modifier 58 may be utilized to indicate that the procedures were staged.) If a diagnosis was established preoperatively, an excision procedure for the purpose of obtaining additional pathologic material is not separately reportable.
Similarly, diagnostic biopsies (e.g., fine needle aspiration, core, incisional) to procure tissue for diagnostic purposes to determine whether an excision or mastectomy is necessary at the same patient encounter may be reported with modifier 58 appended to the excision or mastectomy code. However, biopsies (e.g.,Revision Date (Medicare): 1/1/2014 III-11 fine needle aspiration, core, incisional) are not separately reportable if a preoperative diagnosis exists.
2. The breast procedure codes include incision and closure. Some codes describe mastectomy procedures with ymphadenectomy and/or removal of muscle tissue. The latter procedures are not separately reportable. Except for sentinel lymph node biopsies, ipsilateral lymph node excisions are not separately reportable. Contralateral lymph node excisions may be
separately reportable with appropriate modifiers (i.e., LT, RT).
3. Sentinel lymph node biopsy is separately reportable when performed prior to a localized excision of breast or a mastectomy without lymphadenectomy. However, sentinel lymph node biopsy is not separately reportable with a mastectomy procedure that includes lymphadenectomy in the anatomic area of the sentinel lymph node biopsy. Open biopsy or excision of sentinel lymph node(s) should be reported as follows: axillary (CPT codes 38500 or 38525), deep cervical (CPT code 38510), internal mammary (CPT code 38530). (CPT code 38740(axillary lymphadenectomy; superficial) should not be reported for a sentinel lymph node biopsy. Sentinel lymph node biopsy of superficial axillary lymph node(s) is correctly reported as CPT code 38500 (biopsy or excision of lymph node(s), superficial) which includes the removal of one or more discretely identified superficial lymph nodes. By contrast a superficial axillary lymphadenectomy (CPT code 38740) requires removal of all superficial axillary adipose tissue with all lymph nodes in this adipose tissue.)
4. Breast reconstruction codes that include the insertion of a prosthetic implant should not be reported with codes that separately describe the insertion of a breast prosthesis.
5. CPT codes for breast procedures generally describe unilateral procedures.
6. If a breast biopsy, needle localization wire, metallic localization clip, or other breast procedure is performed withmammographic guidance (e.g., 19281,19282), the physician should not separately report a post procedure mammography code (e.g., 77051, 77052, 77055-77057, G0202-G0206) for the same patient encounter. The radiologic guidance codes include all imaging by the defined modality required to perform the procedure.
Benefits for Mammography Screening – BCBS
Benefits are available for a screening by low-dose mammography for the presence of occult breast cancer for a Participant 35 years of age and older, as shown on your Schedule of Coverage, except that benefits will not be available for more than one routine mammography screening each Calendar Year.
Diagnostic Mammography
A diagnostic mammography is a radiological mammogram and is a covered diagnostic test under the following conditions:
• A patient has distinct signs and symptoms for which a mammogram is indicated;
• A patient has a history of breast cancer; or
• A patient is asymptomatic, but based on the patient’s history and other factors the
physician considers significant, the physician’s judgment is that a mammogram is appropriate.
• Beginning January 1, 2005, Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003, §644, Public Law 108-173 has changed the way Medicare pays for diagnostic mammography. Medicare will pay based on the MPFS in lieu of OPPS or the lower of the actual change.
Billing Requirements – A/B MAC (A) Claims
(Rev. 1519, Issued: 05-30-08, Effective: 05-23-08, Implementation: 06-30-08) A/B MACs use the weekly-updated MQSA file to verify that the billing facility is certified by the FDA to perform mammography services, and has the appropriate certification to perform the type of mammogram billed (film and/or digital). (See §20.1.) A/B MACs (A) use the provider number submitted on the claim to identify the facility and use the MQSA data file to verify the facility’s certification(s). A/B MAC (A) complete the following activities in processing mammography claims:
• If the provider number on the claim does not correspond with a certified mammography facility on the MQSA file, then A/B MACs (A) deny the claim.
• When a film mammography HCPCS code is on a claim, the claim is checked for a “1” film indicator.
• If a film mammography HCPCS code comes in on a claim and the facility is certified for film mammography, the claim is paid if all other relevant Medicare criteria are met.
• If a film mammography HCPCS code is on a claim and the facility is certified for digital mammography only, the claim is denied.
• When a digital mammography HCPCS code is on a claim, the claim is checked for “2” digital indicator.
• If a digital mammography HCPCS code is on a claim and the facility is certified for digital mammography, the claim is paid if all other relevant Medicare criteria are met.
• If a digital mammography HCPCS code is on a claim and the facility is certified for film mammography only, the claim is denied.
NOTE: The Common Working File (CWF) no longer receives the mammography file for editing purposes.
Except as provided in the following sections for RHCs and FQHCs, the following procedures apply to billing for screening mammographies:
The technical component portion of the screening mammography is billed on Form CMS- 1450 under bill type 12X, 13X, 14X**, 22X, 23X or 85X using revenue code 0403 and HCPCS code 77057* (76092*).
The technical component portion of the diagnostic mammography is billed on Form CMS-1450 under bill type 12X, 13X, 14X**, 22X, 23X or 85X using revenue code 0401 and HCPCS code 77055* (76090*), 77056* (76091*), G0204 and G0206.
Separate bills are required for claims for screening mammographies with dates of service prior to January 1, 2002. Providers include on the bill only charges for the screening mammography. Separate bills are not required for claims for screening mammographies with dates of service on or after January 1, 2002. See separate instructions below for rural health clinics (RHCs) and federally qualified health centers (FQHCs).
* For claims with dates of service prior to January 1, 2007, providers report CPT codes 76090, 76091, and 76092. For claims with dates of service January 1, 2007 and later, providers report CPT codes 77055, 77056, and 77057 respectively.** For claims with dates of service April 1, 2005 and later, hospitals bill for all mammography services under the 13X type of bill or for dates of service April 1, 2007 and later, 12X or 13X as appropriate. The 14X type of bill is no longer applicable.
Appropriate bill types for providers other than hospitals are 22X, 23X, and 85X.
In cases where screening mammography services are self-referred and as a result an attending physician NPI is not available, the provider shall duplicate their facility NPI in the attending physician identifier field on the claim.
A/B MACs (B) complete the type of service field in the CWF Part B claim record with a “B” if the patient is a high risk screening mammography patient or a “C” if she is a low risk screening mammography patient for services prior to January 1, 1998.
For services on or after January 1, 1998, the type of service field on CWF must have a value of “1” for medical care (screening) or a “4” for diagnostic radiology (diagnostic). Fill in POS. Fill in deductible indicator field with a “1”; not subject to deductible if screening mammography. Submit the claim to the CWF host. Trailer 17 of the Part B Basic Reply record will give the date of the last screening mammography. The CWF edits for age and frequency for screening mammography. There are no frequency limitations on diagnostic tests or CAD-diagnostic tests. When a screening CAD is billed in conjunction with a screening mammogram and the screening mammogram fails the age or frequency edits then both services will be rejected.
Claims With Dates of Service October 1, 1998 Through December 31, 2001
A radiologist who interprets a screening mammography is allowed to order and interpret additional films based on the results of the screening mammogram while the beneficiary is still at the facility for the screening exam. Where a radiologist interpretation results in additional films, the mammography is no longer considered a screening exam for application of age and frequency standards or for payment purposes. This can be done without an additional order from the treating physician. When this occurs, the claim will be billed and paid as a diagnostic mammography instead of a screening mammography. However, since the original intent for the exam was for screening, for statistical purposes, the claim is considered a screening.
The claim should be prepared for A/B MAC (A) processing reflecting the diagnostic revenue code (0401) along with HCPCS code 76090, 76091, G0204, G0206 or G0236 as appropriate and modifier “-GH” “Diagnostic mammogram converted from screening mammogram on same day.” Statistics will be collected based on the presence of modifier “-GH.” A separate claim is not required. Regular billing instructions remain in place for mammograms that do not fit this situation. A/B MACs (B) should receive a claim for a screening mammogram with CPT code 76092 (screening mammography, bilateral) (Type of Service = 1) but, if the screening
mammogram turns into a diagnostic mammogram, the claim is billed with CPT code 76090 (unilateral) or 76091 (bilateral), (TOS= 4), with the “-GH” modifier. A/B MACs (B) pay the claim as a diagnostic mammography instead of a screening mammography.
NOTE: However, the ordering of a diagnostic test by a radiologist following a screening test that shows a potential problem need not be on the same date of service.
In this case, where additional diagnostic tests are performed for the same beneficiary, same visit on the same day, the UPIN of the treating physician is needed on the A/B MACs (B) claim. The radiologist must refer back to the treating physician for his/her UPIN and also report to the treating physician the condition of the patient. A/B MACs (B) need to educate radiologists and treating physicians that the treating physician’s UPIN is required whenever a physician refers or orders a diagnostic lab or radiology service. If no UPIN is present for the diagnostic mammography code, the A/B MACs (B) will reject the claim
Claims With Dates of Service On or After January 1, 2002, (or On or After April 1, 2002 for Hospitals Subject to OPPS)
A radiologist who interprets a screening mammography is allowed to order and interpret additional films based on the results of the screening mammogram while a beneficiary is still at the facility for the screening exam. When a radiologist’s interpretation results in additional films, Medicare will pay for both the screening and diagnostic mammogram.
A/B MACs (B) Claims
For A/B MACs (B) claims, providers submitting a claim for a screening mammography and a diagnostic mammography for the same patient on the same day, attach modifier “- GG” to the diagnostic mammography. A modifier “-GG” is appended to the claim for the diagnostic mammogram for tracking and data collection purposes. Medicare will reimburse both the screening mammography and the diagnostic mammography.
A/B MAC (A) Claims
A/B MACs (A) require the diagnostic claim be prepared reflecting the diagnostic revenue code (0401) along with HCPCS code 77055* (76090*), 77056* (76091*), G0204, G0206 or G0236 and modifier “-GG” “Performance and payment of a screening mammogram and diagnostic mammogram on the same patient, same day.” Reporting of this modifier is needed for data collection purposes. Regular billing instructions remain in place for a screening mammography that does not fit this situation. Both A/B MACs (A) and (B) systems must accept the GH and GG modifiers where appropriate.
* For claims with dates of service prior to January 1, 2007, providers report CPT codes
76090 and 76091. For claims with dates of service January 1, 2007 and later, providers report CPT codes 77055 and 77056 respectively.
Mammograms Performed With New Technologies
(Rev. 1070, Issued: 09-29-06, Effective: 01-01-07, Implementation: 01-02-07) Section 104 of the Benefits Improvement and Protection Act 2000, (BIPA) entitled Modernization of Screening Mammography Benefit, provides for new payment methodologies for both diagnostic and screening mammograms that utilize advanced new technologies for the period April 1, 2001, to December 31, 2001 (to March 31, 2002 for hospitals subject to OPPS). Under this provision, payment for technologies that directly take digital images would equal 150 percent of the amount that would otherwise be paid for a bilateral diagnostic mammography. For technologies that convert standard film images to digital form, payment will be derived from the statutory screening mammography limit plus an additional payment of $15.00 for A/B MACs (B) claims and $10.20 for A/B MAC (A) (technical component only) claims.
Payment restrictions for digital screening and diagnostic mammography apply to those facilities that meet all FDA certifications as provided under the Mammography Quality Standards Act. However, CAD codes billed in conjunction with digital mammographies or film mammographies are not subject to FDA certification requirements.
Mammography related CAD equipment does not require FDA certification.
Mammography utilizes a direct x-ray of the breast. By contrast, the CAD process uses laser beam to scan the mammography film from a film (analog) mammography, converts it into digital data for the computer, and analyzes the video display for areas suspicious for cancer. The CAD process used with digital mammography analyzes the data from the mammography on a video display for suspicious areas. The patient is not required to be present for the CAD process.
Only one screening mammogram, either 77057* (76092*) or G0202, may be billed in a calendar year. Therefore, providers/suppliers must not submit claims reflecting both a film screening mammography (77057* (76092*)) and a digital screening mammography G0202. Also, they must not submit claims reflecting HCPCS codes 77055* (76090*) or
77056* (76091*) (diagnostic mammography-film) and G0204 or G0206 (diagnostic mammography-digital). MACs deny the claim when both a film and digital screening or diagnostic mammography is reported. However, a screening and diagnostic mammography can be billed together.
* For claims with dates of service prior to January 1, 2007, providers report CPT codes 76090, 76091, and 76092. For claims with dates of service January 1, 2007 and later, providers report CPT codes 77055, 77056, and 77057 respectively.
HCPCS Definition
G0202 Screening mammography producing direct digital image, bilateral, all views
Payment Method:
Payment will be the lesser of the provider’s charge or the amount that will be provided for this code in the pricing file. (That amount is 150 percent of the locality specific technical component payment amount under the physician fee schedule for CPT code 76091, the code for bilateral diagnostic mammogram, during 2001.) Part B deductible does not apply. Coinsurance will equal 20 percent of the lesser of the actual charge or 150 percent of the locality specific payment of CPT code 76091.
HCPCS Definition
G0204 Diagnostic mammography, direct digital image, bilateral, all views
Payment Method:
Payment will be the lesser of the provider’s charge or the amount that will be provided for this code in the pricing file. (That amount is 150 percent of the locality specific amount paid under the physician fee schedule for the technical component (TC) of CPT code 76091, the code for a bilateral diagnostic mammogram.) Deductible is applicable. Coinsurance will equal 20 percent of the lesser of the actual charge or 150 percent of the locality specific payment of CPT code 76091.
NOTE: Effective January 1, 2005, payment will be made under MPFS for claims from hospitals subject to OPPS.
HCPCS Definition
G0206 Diagnostic mammography, direct digital image, unilateral, all views.
Payment Method:
Payment will be made based on the same amount that is paid to the provider, under the payment method applicable to the specific provider type (e.g., hospital, rural health clinic, etc.) for CPT code 76090, the code for a mammogram, and one breast. For example, this service, when furnished as a hospital outpatient service, will be paid the amount under the outpatient prospective payment system (OPPS) for CPT code 76090. Deductible applies. Coinsurance is the national unadjusted coinsurance for the APC wage adjusted for the specific hospital. NOTE: Effective January 1, 2005, payment will be made under MPFS for claims from hospitals subject to OPPS.
HCPCS Definition
G0207 Diagnostic mammography, film processed to produce digital image analyzed for potential abnormalities, unilateral, all views.
Payment Method:
Payment will be based on the same amount that is paid to the provider, under the payment method applicable to the specific provider type (e.g., hospital, rural health clinic, etc.) for CPT code 76090, the code for mammogram, and one breast. For example, this service, when furnished as a hospital outpatient service, will be paid the amount payable under the OPPS for CPT code 76090. Deductible applies. Coinsurance is the national unadjusted coinsurance for the APC wage adjusted for the specific hospital.
Providers bill for the technical portion of screening and diagnostic mammograms on Form CMS-1450 under bill type 13X, 22X, 23X, or 85X. The professional component is billed to the A/B MACs (B) on Form CMS-1500 (or electronic equivalent). Providers bill for digital screening mammographies on Form CMS-1450, utilizing revenue code 0403 and HCPCS G0202 or G0203. Providers bill for digital diagnostic mammographies on Form CMS-1450, utilizing revenue code 0401 and HCPCS G0204, G0205, G0206 or G0207. NOTE: Codes G0203, G0205 and G0207 are not billable codes for claims with dates of service on or after January 1, 2002.
Screening mammograms are covered annually for women 40 years of age and older. The Spanish version of this MSN message should read: El examen de mamografía de cernimiento se cubre una vez al año para mujeres de 40 años de edad o más. For A/B MACs (B) only: For claims submitted with invalid or missing certification number, use the following MSN: MSN 9.2:
This item or service was denied because information required to make payment was missing.
For claims submitted by a facility not certified to perform digital mammograms, the contractor shall use the following remittance advice messages and associated codes when rejecting/denying claims under this policy. This CARC/RARC combination is compliant with CAQH CORE Business Scenario Three.
What is a mammagrom?
Mammography is an x-ray imaging method used to examine the breast for the early detection of cancer and other breast diseases. It is used as both a diagnostic and screening tool.
How does it work?
During a mammogram, a patient’s breast is placed on a flat support plate and compressed with a parallel plate called a paddle. An x-ray machine produces a small burst of x-rays that pass through the breast to a detector located on the opposite side. The detector can be either a photographic film plate, which captures the x-ray image on film, or a solid-state detector, which transmits electronic signals to a computer to form a digital image. The images produced are called mammograms. On a film mammogram, areas of low density, such as fatty tissue, appear translucent (i.e. similar to the black background)., whereas areas of dense tissue, such as connective and glandular tissue or tumors, appear whiter on a black background. In a standard mammogram, both a top and a side view are taken of each breast, although extra views may be taken if the physician is concerned about a particular area of the breast.
What will the results look like?
A radiologist will carefully examine a mammogram to search for areas or types of tissue that look different from normal tissue. These areas could represent many different types of abnormalities, including cancerous tumors, non-cancerous masses called benign tumors, fibroadenomas, or complex cysts. Radiologists look at the size, shape, and contrast of a mass, as well as the edges or margins, which can indicate the possibility of malignancy (i.e. cancer). They also look for tiny bits of calcium, called microcalcifications, which show up as very bright specks on a mammogram. While usually benign, microcalcifications may occasionally indicate the presence of a specific type of cancer. If a mammogram is abnormal, the radiologist may order additional mammogram views, as well as additional magnification or compression, and if suspicious areas are detected, he/she may order a biopsy.
What is digital mammography?
A digital mammogram uses the same x-ray technology as conventional mammograms, but instead of using film, solid-state detectors are used. These detectors convert the x-rays that pass through them into electronic signals that are sent to a computer. The computer then converts these electronic signals into images that can be displayed on a monitor and also stored for later use. Several advantages of using digital mammography over film mammography include: the ability to manipulate the image contrast for better clarity, the ability to use computer-aided diagnosis, and the ability to easily transmit digital files to other experts for a second opinion. In addition, digital mammograms may decrease the need for the re-takes, which are common with film mammography due to incorrect exposure techniques or problems with film development. As a result, digital mammography can lead to lower effective patient x-ray exposures.
In 2005, results from a large clinical trial sponsored by the National Cancer Institute found that digital mammography was superior to film mammography for the following populations[1]
• Women under 50
• Women with dense breasts
• Women who have not gone through menopause or who have been in menopause less than one year
What are the limits of mammography?
For certain types of breasts, mammograms can be difficult to interpret. This is because there is a wide variation in breast tissue density among women. Denser breasts are more difficult to image, and more difficult to diagnose. For this and other reasons, the sensitivity of mammography in detecting cancer can vary over a wide range. For many difficult cases, x-ray mammography alone may not be sufficiently sensitive or accurate in detecting cancer, so additional imaging technologies, such as ultrasound
What are the limits of mammography?
For certain types of breasts, mammograms can be difficult to interpret. This is because there is a wide variation in breast tissue density among women. Denser breasts are more difficult to image, and more difficult to diagnose. For this and other reasons, the sensitivity of mammography in detecting cancer can vary over a wide range. For many difficult cases, x-ray mammography alone may not be sufficiently sensitive or accurate in detecting cancer, so additional imaging technologies, such as ultrasound or magnetic resonance imaging (MRI) may also be used to increase the sensitivity of the exam. Finally, although the majority of abnormal mammograms are false-positives, when cancer is present, early detection can save lives.
Are there risks?
Because mammography uses x-rays to produce images of the breast, patients are exposed to a small amount of ionizing radiation. The risk associated with this dose appears to be greater among younger women (under age 40). However, in some cases, the benefits of using mammography to detect breast cancer under age 40 may outweigh the risks of radiation exposure. For example, a mammogram may reveal that a suspicious mass is benign and, therefore, doesn’t need to be treated. Additionally, if a tumor is malignant and is caught early by mammogram, a surgeon may be able to remove it before it spreads and requires more aggressive treatment such as chemotherapy.Different groups provide different guidelines for mammography. For instance, the American Cancer Society as well as the American College of Radiology recommend that women between the ages of 40 and 49 get mammograms every two years. However, The U.S. Preventive Services Task Force recommends mammograms only for women over age 50. The Task Force states that the benefits of mammography before age 50 do not outweigh the risks.